Lumbar Discectomy
This ultra-minimally invasive endoscopic procedure is performed to remove fragments of a herniated disc in your spine to relieve pressure on adjacent spinal nerves and address pain, numbness, and even weakness in one or both legs.
What Is a Discectomy?
Discs act as spinal shock absorbers. Of the 23 in the spine, 5 are in the lower back. Over time or due to injury, a disc’s outer layer can weaken. This causes the inner material to bulge or herniate, pressing on nerves and causing pain. A discectomy is designed to remove the protruding part to relieve pressure, ease pain, and improve mobility.
Which Conditions Can a Discectomy Address?
Discectomies most commonly address pain related to herniated discs. Common symptoms of a herniated disc include:
- Leg pain that may be accompanied by back pain
- Pain that is felt even when seated
- Numbness, weakness, and/or tingling in one or both legs
Types of Herniated Discs
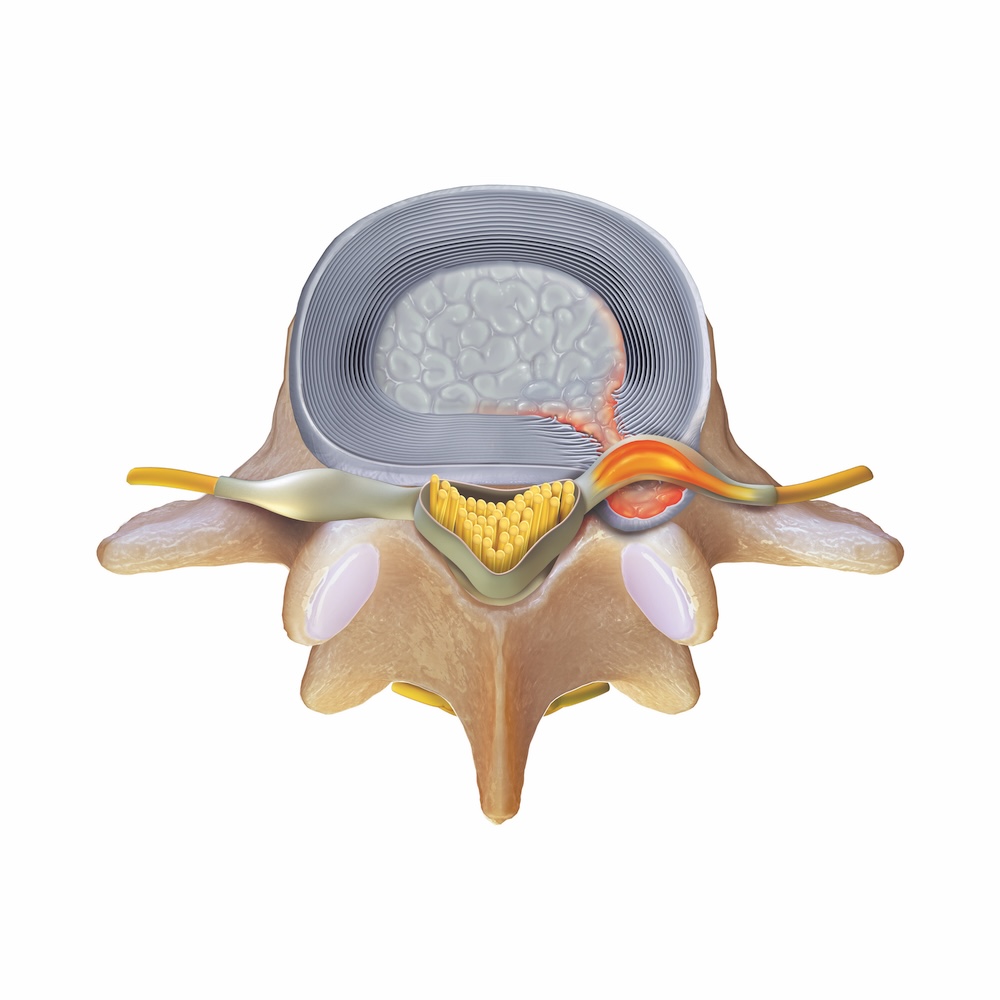

Contained Herniation
Nucleus is bulging or stretching the outer annulus but has not pushed through the annulus wall into the spinal canal
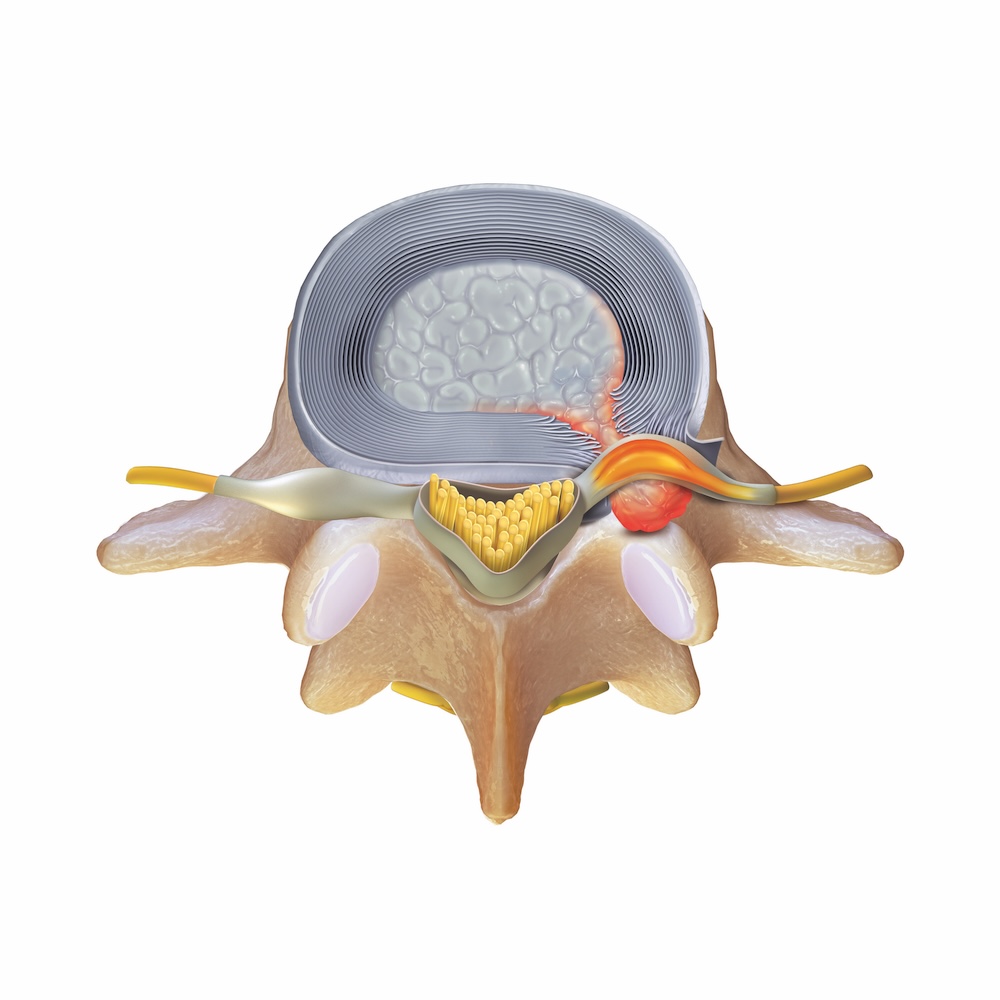
Extruded Herniation
Nucleus has broken through the annulus wall, entering the spinal canal, but is still attached to the main body of the disc
Approaches to Endoscopic Lumbar Discectomy
There are two primary approaches to endoscopic lumbar discectomy: interlaminar and transforaminal.
The interlaminar approach is commonly used to address herniations in the lower area of the lumbar spine, generally at the L4-L5 and L5-S1 levels. The transforaminal approach is commonly used for herniated discs higher in the spine, such as at the L1-L2, L2-L3, and L3-L4 levels, but your surgeon may use this approach at any spinal level depending on the location of your issue as well as your unique anatomy.


Interlaminar Approach
Your surgeon will create a small incision (approximately 1 cm) on the side of the body where the herniation occurred. Using ultra-minimally invasive endoscopic instrumentation, including a spine endoscope and high-resolution camera, they will be able to get a direct view of the herniation. After reaching the disc, your surgeon will remove the herniation, repair the disc, close the wound with a few stitches, and apply an antimicrobial bandage.
Benefits
- Performed through a tiny opening, requiring only a small bandage
- Shown to have fewer complications and allow for a shorter hospital stay compared to open discectomy9
As with all endoscopic spinal surgeries, risks include neurological, vascular, and visceral injuries, recurrence, dysesthesia, and incomplete relief. Additional complications may also occur, including dural tear, hematoma, infection, instability, and facet joint injury.




